Regarding Stroke
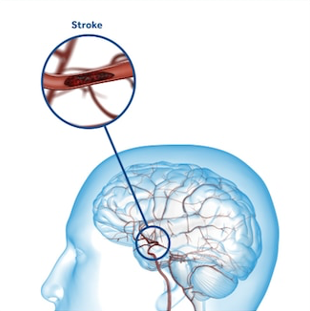
What is stroke?
Stroke occurs when a brain vessel is occluded (ischemic stroke) or ruptured (hemorrhagic stroke). Consequences on patients from an occlusion or rupture of a brain vessel depends on the size and location of the resulting brain lesion.


8% of deaths in Greece are caused by strokes[1]. Despite a reduction in mortality rates per stroke through modern therapies, the aging population leads to an increase in the total number of strokes per year. Recent epidemiological data from the region of Evros estimate the annual incidence of strokes to 587 per 100,000 people, 80% of whom are ischemic[2]. By projecting this rate to the Greek population, the total number of ischemic strokes could be over 50,000 per year.
Stroke Types
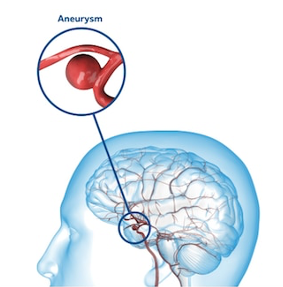
Hemorrhagic strokes may be less common than ischemic strokes but are more severe. The main cause of a brain artery rupture is uncontrolled arterial hypertension. Subarachnoid hemorrhage is a rare cause of hemorrhagic strokes that is caused by a rupture of a brain aneurysm.
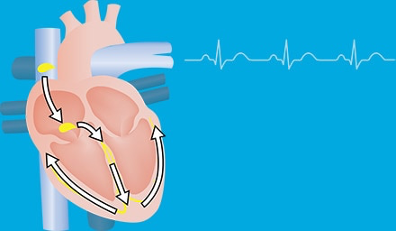
Regular Cardiac rhythm
A small pulse of electricity travels rapidly through the heart to cause muscle contraction.
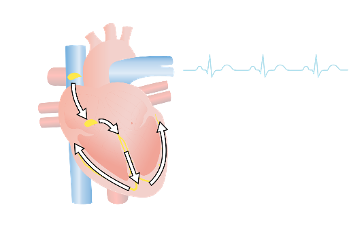
Atrial Fibrillation
In atrial fibrillation, the upper chambers of the heart contract faster than the rest of the heart.
Risk scales
| Risk Factor | Points |
|---|---|
| Congestive heart failure | 4 |
| Hypertension | 2 |
| Age >75 | 2 |
| Vascular disease | 2 |
| Coronary artery disease | 2 |
| Peripheral arterial disease | 1 |
| Obesity (body mass index >30) | 1 |
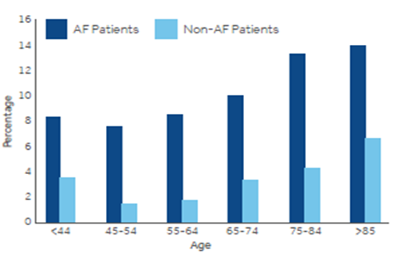
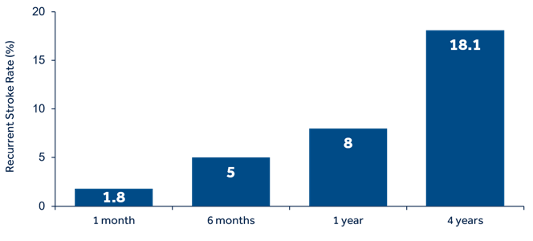
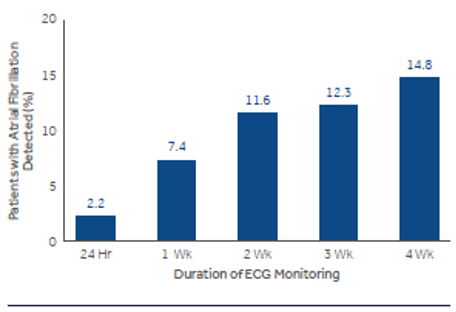
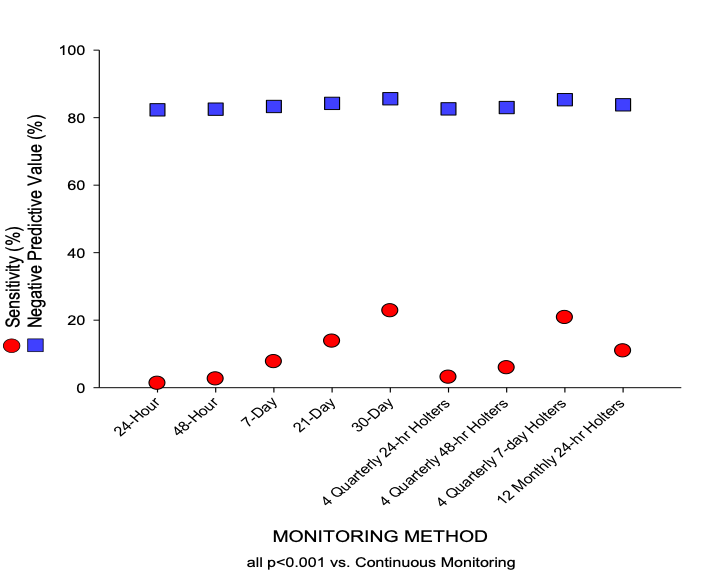
In high-risk patients it is important to prolong ECG monitoring to detect paroxysms of atrial fibrillation, to shift from antiplatelet (common secondary prevention treatment for cryptogenic stroke) to anticoagulation therapy (indicated for secondary prevention of cardioembolic stroke due to atrial fibrillation) in eligible patients[15]. The more we prolong ECG recording the more likely the detection of arrhythmia; best results have been repeatedly reported with implantable devices[10].
[Click here to see the article http://www.hellenicjcardiol-gr.gr/index.php/hjc/article/view/283]
REFERENCES
[1] Wilkins E. et Al. European Cardiovascular Disease Statistics 2017; 2017:192
[2] Tsivgoulis G, et al. Stroke. 2018 Feb;49(2):288-295.
[3] Petty GW, et al. Stroke. 1999;30:2513-2516.
[4] Kolominsky-Rabas PL, et al. Stroke. 2001;32:2735-2740.
[5] Fonseca AC, et al. Eur Stroke J. 2021;6(2):V.
[6] Lee BI, et al. Cerebrovasc Dis. 2001;12:145-151.
[7] Kleindorfer DO, et al. Stroke. 2021;52(7):e364-e467.
[8] Wolf PA, et al. Stroke. 1991;22:983–8.
[9] Kurka N, et al. Stroke 2015; 46: 560 – 563.
[10] Stroke Prevention in Atrial Fibrillation Study. Circulation. 1991;84:527-539.
[11] Tsivgoulis G, et al. J Stroke. 2019;21(3):302-311.
[12] Goudevenos JA, et al. Europace. 1999;1:226-33
[13] Zhao SX, et al. Ther Adv Neurol Disord. 2019;12:1756286419842698.
[14] Kwong, C., et al. Cardiology, 138(3), 133–140.
[15] Writing Group Members, January CT, Wann LS, et al. Heart Rhythm. 2019;16(8):e66-e93.
[16] Choe WC, et al. Am J Cardiol 2015; 6:889–893.
[17] Asaithambi G, et al. J Electrocardiol. 2018;51:973-976.
[18] http://www.hellenicjcardiol-gr.gr/index.php/hjc/article/view/283